— Effect seen with background nusinersen therapy
by
Sophie Putka, Enterprise & Investigative Writer, MedPage Today
February 23, 2024
Some patients with later-onset spinal muscular atrophy (SMA) type 2 and type 3 had improved motor function when the investigational monoclonal antibody apitegromab was added to their treatment, the phase II TOPAZ trial found.
The open-label study had three cohorts. In the first group of ambulatory patients ages 5-21 years who took apitegromab both with and without nusinersen (Spinraza), the mean change from baseline on a revised Hammersmith scale score at 12 months was -0.3 points (95% CI -2.1 to 1.4) and -0.4 (95% CI -3.9 to 3.1), respectively, according to Thomas Crawford, MD, of Johns Hopkins University in Baltimore, and colleagues.
A second cohort with nonambulatory patients ages 5-21 who had adjunctive apitegromab with nusinersen had a mean change of 0.6 points (95% CI -1.4 to 2.7) from baseline on the Hammersmith Functional Motor Scale Expanded (HFMSE).
A third cohort of nonambulatory children 2 years or older — who took either a low or high dose of apitegromab with nusinersen — had mean improvements of 5.3 (95% CI -1.5 to 12.2) and 7.1 (95% CI 1.8-12.5) points on the HFMSE, respectively, the researchers reported in Neurology. Higher scores indicate increased motor function.
“Main takeaways were the strength of the association, particularly in the youngest children,” Crawford wrote in an email to MedPage Today. “We had no way to know which of the three cohorts might show a treatment response.”
For the older ambulatory group, “further work should be done here to see if, and what magnitude, this effect might be when we control for some of the confounders,” Crawford noted.
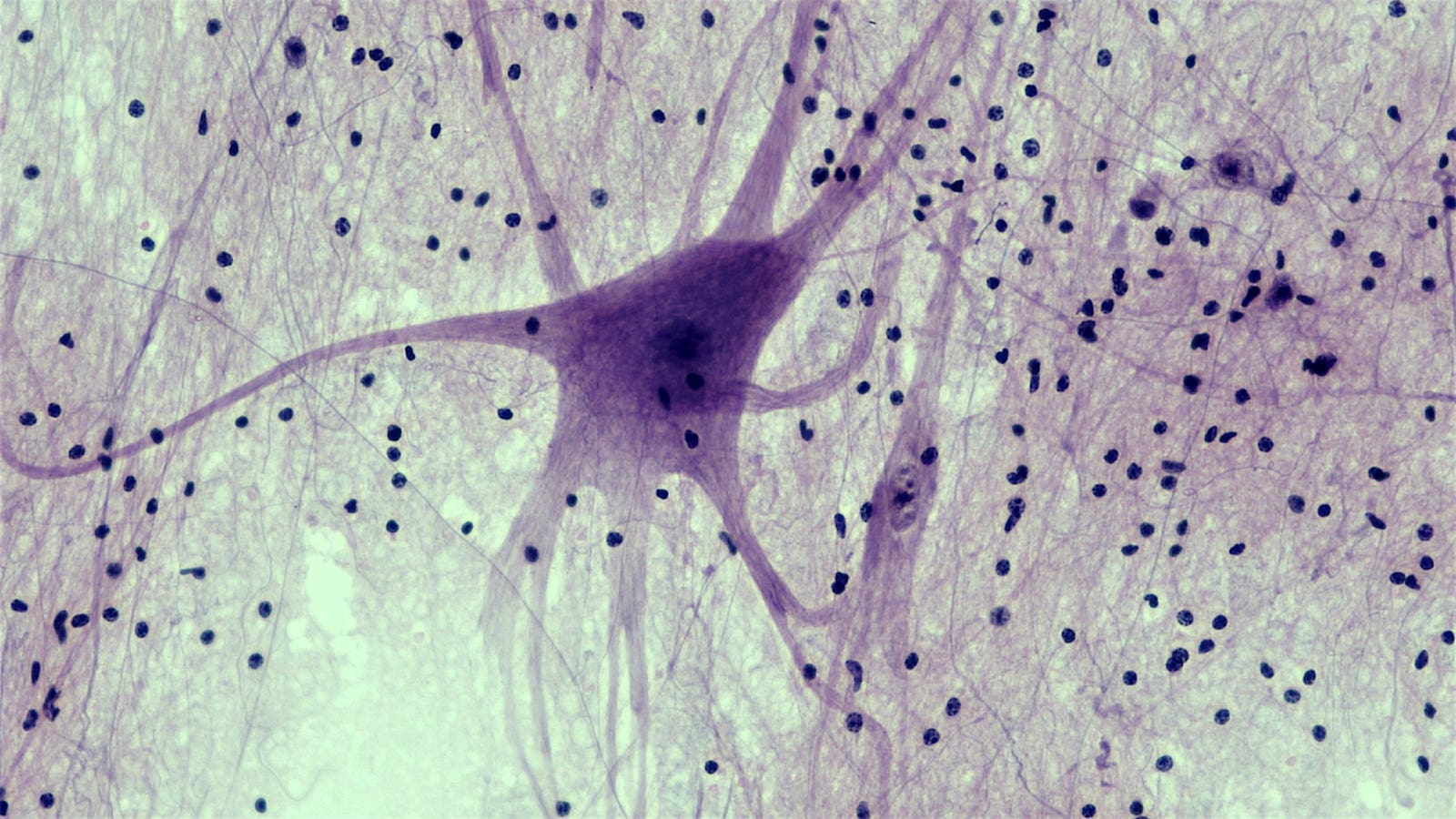
SMA is a neurodegenerative disease caused by homozygous deletions or mutations in the survival motor neuron 1 (SMN1) gene. Nusinersen, which was approved for SMA in 2016, modifies SMN2 pre-messenger RNA splicing, resulting in increased full-length SMN protein levels.
SMA type 1 is the most common and most severe form of the disease. SMA type 2 symptoms start after age 6 months; babies can sit and some can stand with support, but are unable to walk. SMA type 3 symptoms begin after children are age 18 months: children can walk but become progressively weaker and some lose the ability to walk over time.
Apitegromab binds to proforms of myostatin to inhibit the release of active myostatin, which works as a “negative regulator” of skeletal muscle mass, Crawford and colleagues noted. Preclinical studies have suggested that a reduction of myostatin was associated with some improvement in physical function outcomes.
Agents that modify SMN2 like nusinersen have been shown to stop or greatly slow the rate of motor neuron degeneration in SMA. “Apitegromab is best conceived as a means to add additional muscle mass/motor strength to those who have lost power as a consequence of the SMA-associated denervation,” Crawford said.
The TOPAZ study divided 58 patients from 16 sites in the U.S. and Europe with SMA types 2 and 3 into three cohorts. The first cohort, ages 5-21 years, had ambulatory SMA type 3 and took apitegromab alone or with nusinersen in two arms. The second, also ages 5-21, had nonambulatory SMA type 2 or 3, and took both drugs. The third, ages 2 years or older, had nonambulatory SMA type 2, and took both drugs in two arms, 2 mg/kg and 20 mg/kg.
All participants took apitegromab every 4 weeks via infusion for 12 months. Participants had been treated with nusinersen for a mean of 25.9 months (mean of nine doses) before enrollment.
The average age of the cohorts was around 12-13 years old in cohort 1, 11.7 in cohort 2, and around 4 in the third cohort. Most groups included at least 50% females except the 2 mg/kg apitegromab group, which had 70% males.
No deaths were reported in the trial, and the most common treatment-emergent adverse events were headache, pyrexia, upper respiratory tract infection, cough, and nasopharyngitis. Five unrelated serious adverse events were also reported.
Limitations included the study’s open-label design, the researchers acknowledged. In addition, it was difficult to distinguish benefits from background therapy versus the intervention, or between normal development and development while on treatment.
The double-blind placebo-controlled phase III SAPPHIRE trial is underway to investigate apitegromab in nonambulatory type 2 and 3 SMA patients treated with nusinersen or risdiplam (Evrysdi), an SMN2 pre-mRNA splicing modifier approved for SMA in 2020.
-
![author['full_name']](https://clf1.medpagetoday.com/media/images/author/Putka_Resize_96.jpg)
Sophie Putka is an enterprise and investigative writer for MedPage Today. Her work has appeared in the Wall Street Journal, Discover, Business Insider, Inverse, Cannabis Wire, and more. She joined MedPage Today in August of 2021. Follow
Disclosures
Funding for the trial came from Scholar Rock.
Crawford reported relationships with AveXis/Novartis, Biogen, Pfizer, and Roche/Genentech.
Co-authors reported multiple relationships with industry.
Primary Source
Neurology
Source Reference: Crawford TO, et al “Safety and efficacy of apitegromab in patients with spinal muscular atrophy types 2 and 3” Neurology 2024; DOI: 10.1212/WNL.000000000020915.
Leave a Reply