— Evidence is improving for management of this extra-rare autoimmune disease in kids
by
Crystal Phend, Contributing Editor, MedPage Today
December 22, 2023
Generalized myasthenia gravis (gMG) is a rare condition, especially in youth. However, evidence is beginning to accrue for management of juvenile cases.
Prevalence increases with age. Fully 65% of cases were in adults 65 and older, according to a recent study of epidemiology of gMG using the Clarivate Real-World Data Repository of claims and electronic healthcare records covering most U.S. health plans for 2016-2021.
Just 1.2% of cases were in children under 18. Previous studies have estimated a prevalence of 3.6 to 13.8 per million among pediatric patients. Females accounted for a somewhat higher proportion of cases that occur before age 50.
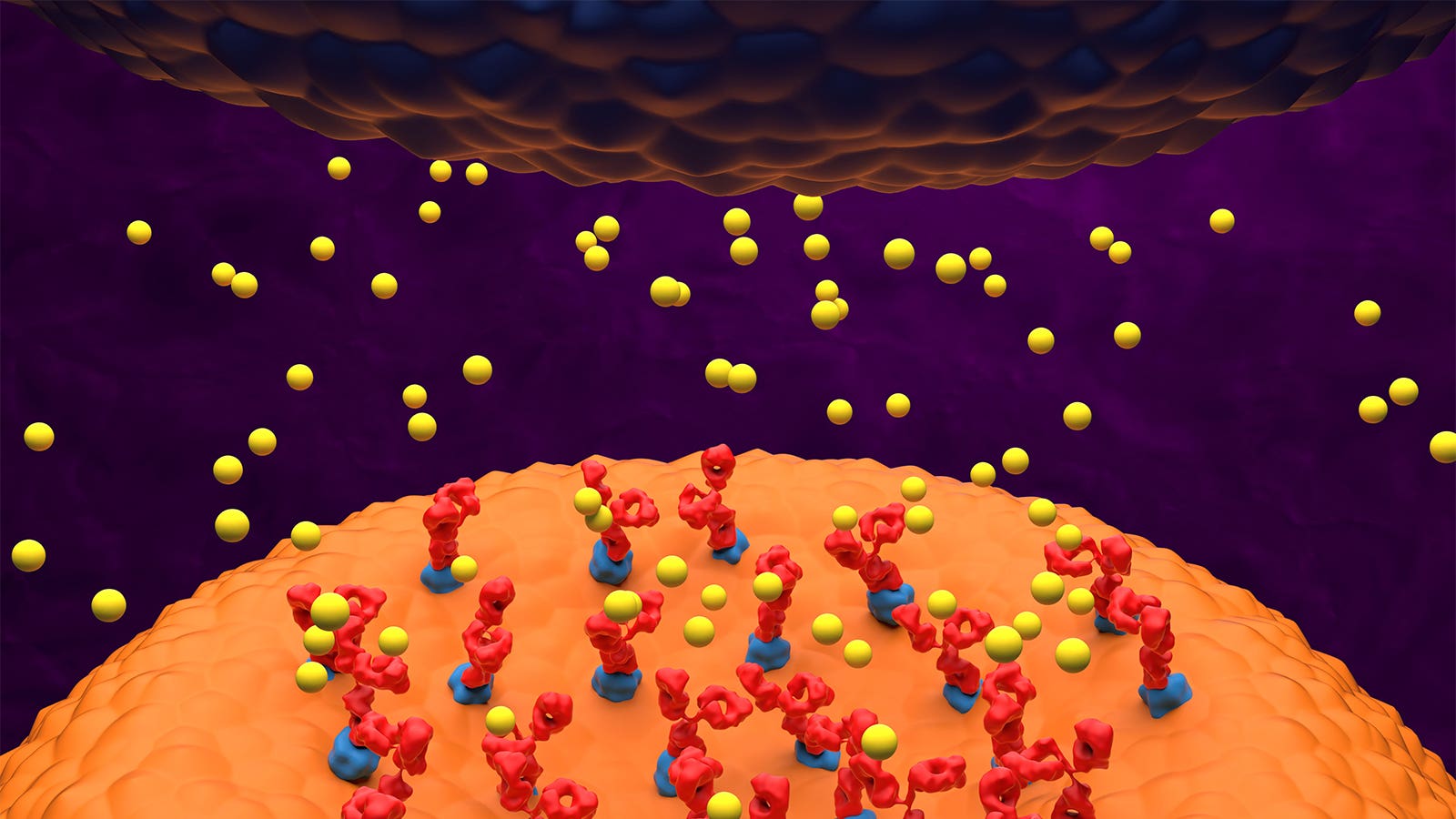
Childhood cases are often classified as juvenile myasthenia gravis, which is more variable in presentation and more difficult to diagnose. Prepubertal children with gMG have a lower frequency of acetylcholine receptor antibodies, but their disease must be differentiated from congenital myasthenic syndromes, which do not have an autoimmune basis.
Clinical features are distinct from adult MG in that children more often have isolated ocular symptoms and higher probability of remission.
“Treatment commonly includes anticholinesterases, corticosteroids with or without steroid-sparing agents, and newer immune modulating agents,” noted a review in Autoimmune Diseases. “Plasma exchange and intravenous immunoglobulin (IVIG) are effective in preparation for surgery and in treatment of myasthenic crisis. Thymectomy increases remission rates.”
These newer immune-modulating drugs are starting to be prospectively studied in pediatric use.
Complement inhibitor eculizumab (Soliris), the first in a spate of drug approvals for adult gMG in recent years, met its primary and all secondary efficacy endpoints in an open-label, single-arm trial among 11 adolescents ages 12 to 17 years with refractory anti-acetylcholine receptor (AChR) antibody-positive gMG, reported in April in Neurology. Weight-based dosing improved Quantitative Myasthenia Gravis total score by an average 5.8 points and MG-Activities of Daily Living (MG-ADL) total score by 2.3 points, both significant compared with baseline at 26 weeks. The treatment was well tolerated, with mild to moderate treatment-emergent adverse events, predominantly unrelated to the study drug, and no meningococcal infections.
The results were “no different than the adults,” senior author James Howard Jr., MD, of the University of North Carolina at Chapel Hill, told MedPage Today.
That trial led to approval for children ages 6 to 17 years in the European Union and Japan. Drugmaker AstraZeneca has announced that regulatory submissions are underway with other health authorities as well.
“We don’t believe that adolescent- or pediatric-onset myasthenia gravis is necessarily any different from an immunologic perspective compared to adult patients,” said Richard Nowak, MD, director of the Yale Myasthenia Gravis Clinic in New Haven, Connecticut. “There probably are some nuances and some differences that we don’t really have a good clear handle on,” but the mechanisms of the complement and neonatal Fc receptor inhibitors should work the same for AChR antibody-positive cases regardless of whether onset is in childhood or adulthood.
However, there is a potentially greater role for those drugs based on their side effect profile compared with older therapies, such as corticosteroids, “especially in someone that’s growing” due to risk of stunting, he said.
Howard noted that while pediatric trials are “exceptionally difficult to perform” in this rare condition, a number of others are in the design phase or underway with other newer immunomodulating agents.
Aside from the rarity of the condition, it’s difficult to get accurate assessments with current measures in children younger than 12, he pointed out.
Carolina Barnett-Tapia, MD, PhD, of the University of Toronto Prosserman Centre for Neuromuscular Diseases, agreed.
“The truth is, we know for many diseases and conditions that you need children-specific measures,” she said. “Diseases may manifest differently in children; and [for] some things, children are not little adults, they do different things.”
For example, the MG-ADL tool used in most adult trials asks patients whether they have difficulty washing or brushing their hair or brushing their teeth, “but most children don’t care at all whether they can brush their hair or their teeth,” Barnett-Tapia told MedPage Today. “Children probably are more interested if they can play, they can run with their peers, I guess use an iPad.”
While modifying the adult scales might be one way forward, there are efforts to develop a pediatric-specific scale for MG, she noted.
Also, the Pediatric Myasthenia Gravis Consortium has established a registry for patients diagnosed before age 18 (even if currently an adult) with congenital or acquired disease from six pediatric centers across the U.S.
“You really need a registry to have large numbers to understand better the natural history of the disease in children,” Barnett-Tapia said. “They’re doing that.”
Disclosures
Howard disclosed research funding to his institution from Alexion AstraZeneca Rare Disease, argenx, Cartesian Therapeutics, the CDC, the Myasthenia Gravis Foundation of America, the Muscular Dystrophy Association, the NIH, the Patient-Centered Outcomes Research Institute, Ra Pharmaceuticals/UCB Bioscience, and Takeda, as well as honoraria or consulting fees from Academic CME, Alexion AstraZeneca Rare Disease, argenx, Biologix Pharma, F. Hoffmann-LaRoche, Horizon Therapeutics, Medscape CME, EMD Serono, NMD Pharma, Novartis, PeerView CME, PlatformQ CME, Regeneron, Sanofi, and Zai Labs.
Nowak disclosed grant or research support from the NIH, the Myasthenia Gravis Foundation of America, Grifols, Alexion, Genentech, argenx, Ra Pharma (now UCB), Momenta (now Janssen), Immunovant, Annexon, and Viela Bio (now Horizon Therapeutics), as well as consulting or advisory relationships with Alexion, Cabaletta, Cour Pharmaceuticals, Ra Pharma, Momenta, argenx, Immunovant, and Viela Bio.
Barnett-Tapia disclosed advisory board membership for argenx, Alexion, UCB, Janssen, AstraZeneca, and Sanofi, as well as grant support from the Department of Defense, the NIH, Muscular Dystrophy Canada, the Myasthenia Gravis Rare Disease Network, Grifols, and Octapharma. She is the primary developer of the Myasthenia Gravis Impairment Index.
![author['full_name']](https://clf1.medpagetoday.com/media/images/author/crystalPhend_188.jpg)
Leave a Reply